
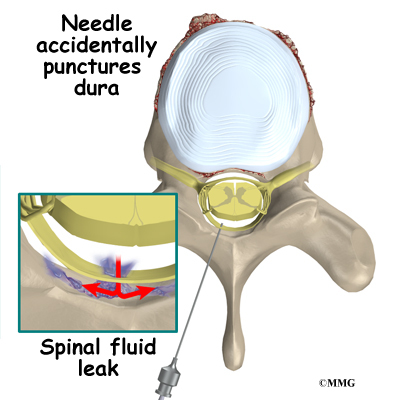
The spinous process, bilateral lamina and facet joints were exposed layer by layer. See Table 1 for details.Īll operations were performed under general anaesthesia, in the prone position and via the posterior median approach. The follow-up time ranged from 6 to 30 months (mean: 15.7 ± 6.3 months). There were 2515 cases of primary surgery and 664 cases of revision surgery. There were 1660 cases of total lamina decompression and 1519 cases of window decompression. There were 807 cases of LDH, 1143 cases of LSS, 1122 cases of LS, 93 cases of LDS, and 14 cases of LST. The subjects’ ages ranged from 24 to 80 years (mean: 56.3 ± 12.8 years). A total of 3179 patients met the inclusion criteria, including 1606 males and 1573 females 2058 of these patients (1435 males, 523 females) had a history of smoking. Reddish bloody fluid or clear fluid accumulated subcutaneously after the incision.Ī total of 3840 patients who underwent lumbar posterior surgery in our hospital from January 2019 to December 2020 were selected as the research subjects 661 patients were excluded by exclusion criteria. The incision had reddish blood or clear fluid exudation.Ī large amount of reddish bloody fluid or clear fluid was drained from the drainage tube or incision after surgery. Postoperative headache, dizziness, and vomiting were related to the patient’s position. There was a present or past history of mental illness.ĭural injury or CSFL was confirmed during the operation. Patients or their families had poor compliance and were unwilling to cooperate with the treatment and follow-up visits. Malignant tumours were present in the lumbar spinal canal. Patients underwent cervical and thoracic surgery at the same time. Patients and their families had good compliance and were willing to cooperate with the treatment and follow-up visits. Posterior lumbar decompression (total lamina decompression or fenestration decompression) was present. There were no obvious surgical contraindications. There were unsatisfactory results after systematic conservative treatment for more than 3 months. Once appear, CSFL can also be effectively dealt without obvious adverse reactions after intraoperative effectively repair dural, head down, adequate drainage after operation, the high position, rehydration treatment, and other treatments.īased on the patients' medical history, signs and imaging examinations, they were diagnosed with lumbar disc herniation (LDH), lumbar spinal stenosis (LSS), lumbar spondylolisthesis (LS), lumbar degenerative scoliosis (LDS), or lumbar spinal benign tumour (LST). Effective prevention were the key to CSFL in lumbar surgery. Type of disease, preoperative epidural steroid injection, number of surgical levels and revision surgery were the risk factors for CSFL. Age, type of disease, duration of disease, preoperative epidural steroid injection, number of surgical levels and revision surgery had effects on CSFL ( P 0.05). The incidence of 115 cases with cerebrospinal fluid leakage, was 3.6% (115/3179).One-way ANOVA showed that gender, body mass index (BMI), smoking history, combined with type 2 diabetes and surgical method had no significant effect on CSFL ( P > 0.05). Data of gender, age, body mass index(BMI), duration of disease, diabete, smoking history, preoperative epidural steroid injection, number of surgical levels, surgical methods (total laminar decompression, fenestration decompression), revision surgery, drainage tube removal time, suture removal time, and complications were recorded. There were 807 cases of lumbar disc hemiation (LDH), 1143 cases of lumbar spinal stenosi (LSS), 1122 cases of lumbar spondylolisthesis(LS), 93 cases of lumbar degenerative scoliosis(LDS),14 cases of lumbar spinal benign tumor (LST). MethodsĪ retrospective analysis was performed on 3179 patients with CSFL strategies lumbar posterior surgery in our hospital from January 2019 to December 2020. To analyze the risk factors of cerebrospinal fluid leakage (CSFL) following lumbar posterior surgery and summarize the related management strategies.


 0 kommentar(er)
0 kommentar(er)
